The Science behind ClearPoint® Acne Supplements by LEROSETT®
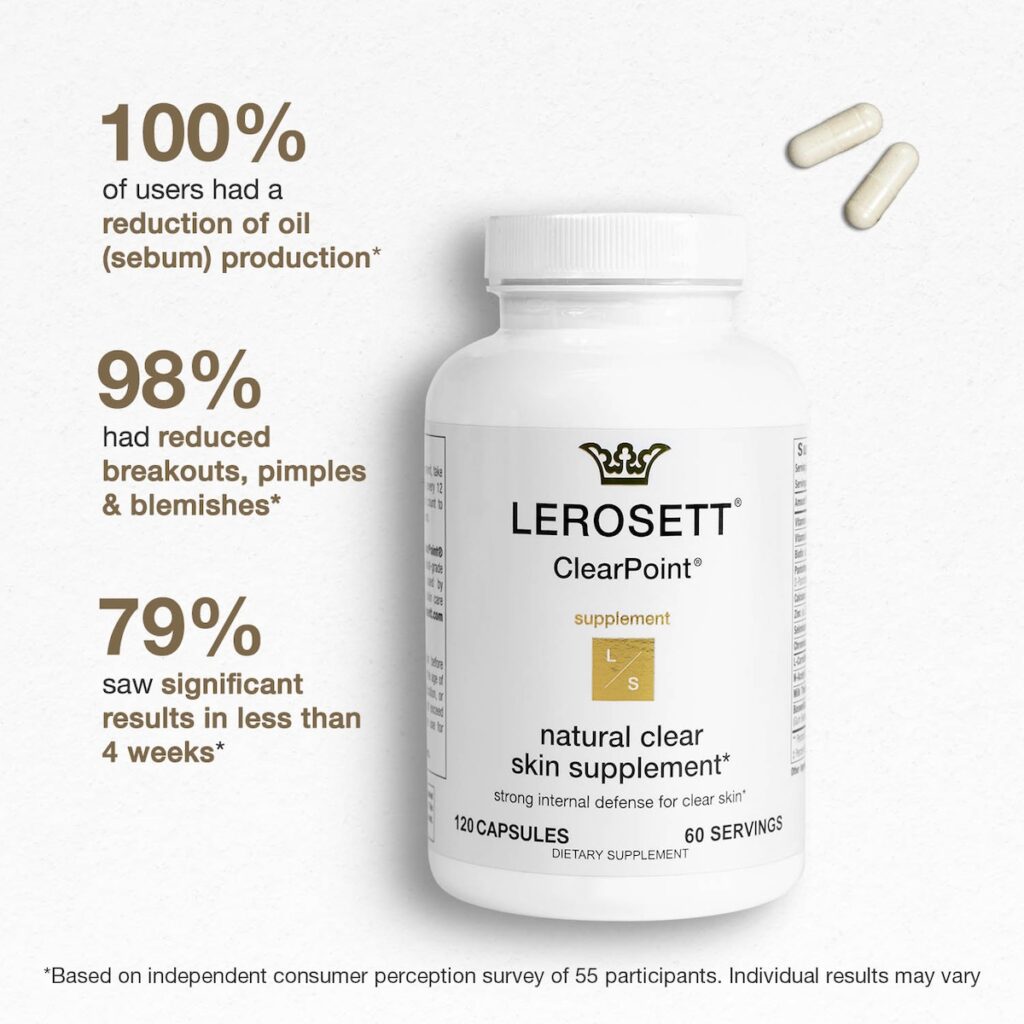

Don’t let acne hold you back any longer – try ClearPoint® by LEROSETT® today and see the difference for yourself!
Transform your skin with ClearPoint®, the powerful supplement developed in Sweden after years of research to treat acne, oily skin, inflammation, irritation, and breakouts from the inside out. ClearPoint® uses a precise blend of ingredients that target the root cause of pimples, oily skin, and acne, allowing you to achieve clear, smooth skin. It slows down your body’s oil (sebum) production, preventing pimples and breakouts from forming while increasing the production of Coenzyme A to help break down excess oils in the skin. ClearPoint®’s unique combination of Pantothenic acid, L-carnitine, Zinc, Selenium, Calcium, Botswella serrate, and other botanical ingredients make it the most effective formula for treating acne.
Back to ClearPoint® Order Page
“A Medical Hypothesis” by Lit-Hung Leung, M.D This research originally appeared in the Journal of Orthomolecular Medicine Vol. 12 Number 2, 1997. Below is a condensed version of the study and research by Gunilla of Sweden® highlighting the more pertinent factors relating to LEROSETT® ClearPoint® All Natural Clear Skin Supplements.
Each vitamin, mineral, and amino acid used in ClearPoint® Clear Skin Supplements are safe & work synergistically, managing oil (sebum) production and preventing pimples from forming.
When natural Coenzyme A is not in balance, lipids accumulate in the sebaceous glands, sebum excretion increases, and acne appears.
Vitamin A (as Retinol Acetate) (2500IU) 750mcg
Vitamin A is a fat-soluble vitamin, meaning once it’s been stored in fat cells in the body, it remains there. That can be dangerous if there is too much in the body, but the lack of Vitamin A is a cause of pimples. It is added to this best acne treatment for teens and adults at a safe yet effective dose to help treat zits, pimples & blemishes.
Vitamin B3 (as Niacinamide) 25mg
Vitamin B3, known as Niacin, is commonly found in food sources such as fish, meat, eggs, green vegetables, and beans. Niacin also helps absorb important proteins needed to combat and prevent breakouts.
Biotin (as D-Biotin) 150mcg
Biotin is a water-soluble vitamin crucial for preventing pimples. It works synergistically with the other B-vitamins in LEROSETT® Clear Skin Supplements and is vital for creating a protective barrier of fatty acids that defend our skin.
Pantothenic Acid (as Calcium D-Pantothenate) 750mg
Vitamin B5, also known as Pantothenic Acid, is a water-soluble vitamin indicating it can be consumed safely at large doses as any remainder of the vitamin will be excreted. Vitamin B5 in this vitamin for hormonal acne has been proven effective at managing hormonal pimples as it reduces the number of sebum or oil produced in the skin. Overactive oil glands are a factor in breakouts and can be caused by a loss of pantothenic acid. (Calcium used is in the form of Calcium D-Panthonate)
Calcium (as Calcium D-Pantothenate) 64mg
Calcium pantothenate is the calcium salt of the water-soluble vitamin B5 (pantothenic acid), ubiquitously found in plants and animal tissues with antioxidant properties.
Zinc (as Zinc Aspartate) 10mg
While zinc is thought to help keep you healthy by reducing illnesses, it’s been studied for many other medical concerns, including acne and skin problems. Zinc is one of the most widely studied forms of acne treatment. Zinc minimizes inflammation and redness, primarily when used with Selenium.
Selenium (as Selenomethionine) 100mcg
Selenium is a powerful antioxidant that helps strengthen our immune system by attacking bacteria that produce zits. When mixed with a specific dose of Vitamin A, it is highly effective at treating blemishes. The result of Selenium is to relieve inflammation and redness from pimples.
Chromium (as Chromium Polynicotinate) 60mcg
A cause of breakouts is fluctuating blood sugar levels due to a diet high in sugar, high¬glycemic carbohydrates, and trans fat. Chromium is essential for regulating blood sugar which will help keep our hormones from wavering and preventing hormonal blemishes. Chromium will also stop bacteria from spreading to other pores in our skin.
L-Carnitine L-Tartrate 250mg
The body naturally uses L-Carnitine to move oils to Coenzyme-A glands. But your body usually doesn’t have enough L-Carnitine to deal with excess oil. Therefore we add L-Carnitine to increase the effectiveness of Pantothenic Acid.
Boswellia Serrata (65% Boswellic Acid) 40mg
We use Boswellia for the herb’s anti-inflammatory effect. Boswellia has traditionally been used in acne therapy, and we have found great success with the exact amount combined with Selenium.
Proprietary Blend: 200mg
Green Tea Extract: Research has shown both oral and topical use of green tea to treat acne effectively.
Maca Root Powder (Lepidium meyenii): Helps keep hormones in check—a bonus for those who experience acne flare-ups around that time of the month.
Milk Thistle Seed Extract (4:1): Milk thistle helps reduce acne by boosting the body’s natural mechanisms, such as glutathione.
Turmeric Root Powder: contains curcuminoid, a compound with anti-inflammatory, antimicrobial, and antioxidant properties.
Understanding that people respond to supplements differently and should always consult a physician before using any supplement or vitamin is essential. Also, even the best supplement can’t remove the dead skin cells that clog your pores; you still need an effective acne cleanser and maybe a spot treatment for an occasional pimple that can break through.
Over the years the pathogenesis of acne vulgaris has been extensively studied including, the structure and function of the pilosebaceous follicle, the physiology of sebum, microflora in acne vulgaris, and abnormal follicular keratinization, considered to be one of the earliest events in acne formation. Despite the concerted effort of many scientists, internists, pathologists, and dermatologists, the pathogenesis of acne vulgaris remains mostly elusive. In this paper, I would like to approach this problem from a different perspective. My clinical observations suggest that acne vulgaris may be closely related to the consumption of diets, which are rich in fat content. This impression is by no means novel. Textbooks do briefly mention this correlation though, more often than not, it is dismissed as irrelevant. However, my observations have led to quite the contrary conclusions. Not only is the fat content of food closely related to acne vulgaris but it forms some sort of linear relationship with the disease process. The more fat the patient consumes, the more severe will be the acne process. This observation is in line with the opinion of many dermatologists that chocolate, which is composed mainly of the creamy part of milk and has a high degree of fat content, is bad for acne. Significantly, in this group of patients, any deliberate attempt in trying to avoid a fatty diet over a period of weeks, if not days, will often result in an important compound, cholesterol, which in turn is primarily synthesized from units of acetyl-CoA. In the synthetic process, the body naturally is always trying not only to reach for a healthy level of androgens but an optimal level, to allow the body to function at its best. However, this is not always possible, and the average level reached may not represent the optimal level. This is nature’s flexible way of dealing with a shortage of essential dietary elements in any form to achieve a level that is just enough to manage the present situation, leaving a variable degree of deficiency from the optimal level. In the current instance, in the two groups of boys, one group may have a reasonable level of androgens that is falling short of the optimum. One possible explanation for this is that there is a lack of basic building blocks, the acetyl-CoAs, which deter the body from operating at peak efficiency. If this is a viable possibility, it suggests that a plentiful supply or a deficiency of acetyl-CoA in the body may play a role in the acne process. This is certainly possible. Aside from its role in the synthesis of the sex hormones, acetyl-CoA, of which Coenzyme-A is the vital component, it is also essential in fatty acid metabolism as an acyl carrier in the lengthening and degradation of long chain fatty acids by adding or removing acyl groups in the metabolic process. Acne vulgaris is related to lipid metabolism as well as the sex hormones, both of which have a lot to do with Coenzyme A. This relationship provides a reasonable ground to link up the acne process to Coenzyme A and to investigate the pathogenesis of acne vulgaris along this line.
In trying to link acne vulgaris to Coenzyme-A, it is important to have a hypothesis supporting some basic facts. A closer look at Coenzyme-A may provide the evidence. A Sharing scenario; as a coenzyme active in both fatty acid metabolism and sex hormone synthesis, Coenzyme-A is shared between two different metabolic processes. This is not uncommon in biochemical reactions in metabolism, where a coenzyme is often shared among a number of reactions. Coenzyme-A is arguably the most important coenzyme in the body, and when a coenzyme is involved in the metabolic process to such an extent as this, it becomes legitimate to ask if a shortage and deficiency is possible. To answer this, a brief look at the structure of Coenzyme-A is warranted. Pantothenic Acid; Coenzyme-A is formed from adenosine triphosphate, cysteine, and pantothenic acid. These pantothenic acids are the only components that are vitamin and must be provided from our dietary intake. Could there be an insufficient intake of pantothenic acid resulting in a deficiency in Coenzyme-A, which would leave the body unable to cope with all the reactions, that it has to perform with that all-important coenzyme? Conventional wisdom does not think so. It is suggested that pantothenic acid, being ubiquitous, can be had from whatever kind of food that is taken in and that there is no question as to its deficiency in our body. However, a deficiency is still possible. After all, when so many reactions are dependent on the same agent, its demand must be tremendous. Shortage under such circumstances is not entirely impossible.
If the question of deficiency of Coenzyme-A does come up, how does it affect acne, knowing its importance in fatty acid metabolism and sex hormone synthesis? This is the crucial question. This is where the new hypothesis on the pathogenesis of acne vulgaris is based, and this is where it diverges from conventional medical ideas. The author’s proposed hypothesis for the pathogenesis of acne vulgaris is that the disease process is not caused by androgens or any other sex hormones, but instead, the disease process results from a defect in lipid metabolism that is secondary to a deficiency in pantothenic acid, hence Coenzyme-A. Coenzyme-A, in carrying out its function efficiently both as an agent in fatty acid metabolism and an agent in androgen and sex hormone synthesis, has to be present in sufficient amounts, and anything less than sufficient will result in some compromise.
Faced with the dilemma of a shortage of Coenzyme-A the body will tend to make a choice that is to the best advantage of the individual. The body does so by mostly maintaining the functionally more important reaction, while at the same time slowing down the lesser important one. The choice here is a relatively simple one. Nature will seek to take care of the synthesis of hormones first because the continuation of the species depends on the development of the sex organs. Fatty acid metabolism is, for the time being, at least in part halted. Lipids start to accumulate in the sebaceous glands, sebum excretion is increased, and acne begins to appear. When there is enough Coenzyme-A in the body, however, both reactions will be well taken care of. There are enough sex hormones for the sex organs to develop. The lipids in the sebaceous glands are entirely metabolized by sufficient Coenzyme-A, and there will be no unwanted lipid in the glands, and little sebum will be excreted to cause acne vulgaris.
The mechanism proposed above may be the reason why two groups of adolescent boys both with a normal blood level of androgen may exhibit differences in the incidence of acne. The group with acne is the one that has not enough pantothenic acid in the body, whereas in the other group, pantothenic acid levels are not deficient. This new theory seems to work well here, and can be tested in other metabolic situations. In the case in which endogenous androgen stimulates acne, whereas exogenous does not, the reasoning for the observation is the same. Any endogenous androgen synthesis will require the participation of extra amount of pantothenic acid. This will channel off some of those that are doing the work of fatty acid metabolism. Consequently, fatty acid metabolism becomes less efficient and the individual is more prone to have acne. Today, the percentage of adult women that have acne is increasing. Some of these women may not have had acne as teenagers, and are surprised to find that they have to deal with this unpleasant problem during their adult years. Acne can have profound psychological and social effects on adults, just as it does in teenagers.
Microcomedo Acne vulgaris of adulthood is similar to teenage acne. The pilosebaceous units of the face, chest, and back can be involved. The primary lesion of acne is the “microcomedo.” A microscopic plug develops due to the presence of thickened and impacted keratin (dead cells) and excess oil production (sebum). More and more of the keratin and sebum back up behind this plug and form a distended follicular pore. This results in either an open comedo (blackhead) or a closed comedo (Whitehead). The enlarged pilosebaceous structure allows Propionibacterium acne’s, an anaerobic diphtheroid, to increase. Propionibacterium acne’s contributes to the breakdown of lipids to free fatty acids, which are highly inflammatory. The distended follicle can rupture, causing further inflammation and the development of papules, pustules, and nodules.